EECP? is a Non-Invasive treatment for patients with refractory angina and heart failure.

Patients are usually treated with EECP one hour a day, six days a week for six weeks for a total of 35 hours. In some patients it can be offered two hours per day.
Patients Receiving EECP
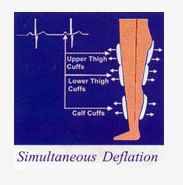
Cuffs inflate sequentially from the calves to the upper thighs and buttocks to raise diastolic coronary perfusion pressure and increase venous return. Cuffs deflate at the onset of systole producing left ventricular unloading with an associated decrease to cardiac workload.Acute Hemodynamic Effects.
The acute hemodynamic effects of external counterpulsation are similar to those seen with an intra-aortic balloon pump with the addition of increased venous return.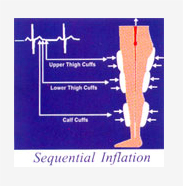
Inflation resulted in:
- Increase central aortic diastolic pressure up to 92%
- Increase intracoronary diastolic pressure up to 93%
- Increase in coronary perfusion pressure.
- Increase coronary collateral flow velocity.
- Increase venous return and therefore preload.
- Increase in cardiac output up to 25%
Deflation resulted in:
- Decrease central aortic systolic pressure up to 11%
- Decrease intracoronary systolic pressure up to 15%
- Decrease in LV end-diastolic pressure up to 25%
- Reduce systemic vascular resistance.
- Decrease Left ventricular workload and afterload.
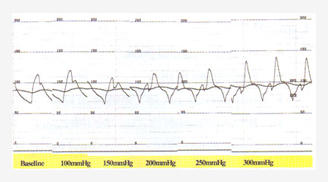
Intracoronary tracing in catheterization Lab showing gradual increase in cuff inflation pressure resulting in increase diastolic pressure, mean arterial pressure and decrease systolic pressure
Must – EECP
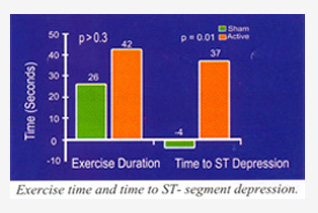
The MUST – EECP trail is a randomized, controlled, double-blinded, multi-center trail undertaken at seven leading university hospitals in the United States. Patients in the active EECP group demonstrated significantly increased in exercise duration and statistically significant increased in time to exercise-induced ST-segment depression when compared to sham group from baseline.Clinical Benefits.
- Relief of anginal pain.
- Reduction in the use of nitrates.
- Improvements in Quality of life.
- Improvements in Exercise tolerance.
- Clinical benefits are sustained for up to 5 years following treatment.
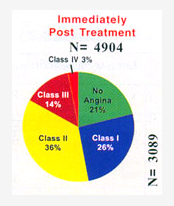
International EECP Patient Registry (IEPR)
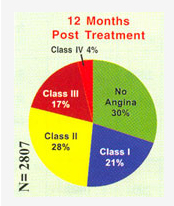
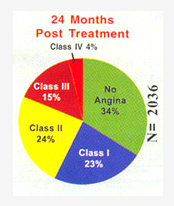
In 1998, the International EECP Patient Registry (IEPR) was established. The IEPR is a voluntary registry of consecutive patients open to provider members. Additionally, an analysis of long-term outcomes suggests that the clinical benefits achieved are sustained up to two years following an initial course of treatment.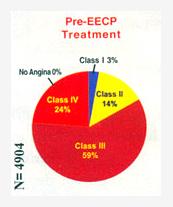
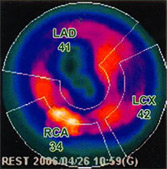
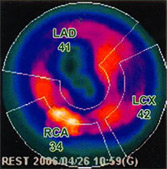
EECP has shown to improve the myocardial perfusion to the ischemic area. It is assessed by PET and SPECT Nuclear study. The Mechanism is believed to be increase pressure gradient and coronary blood flow velocity in coronary vascular bed. This will lead to formation of new vessels and opening of the dormant collaterals. EECP treatment has shown to increase the plasma nitric oxide and decreases the Endothelin level. These changes were proportional to the treatment duration and were sustained even after completion of the treatment.
| Mean Age | 66.9yrs | Prior Mi | 67.6% |
| Duration of CAD | 10.9yrs | CHF | 31.7% |
| Prior PCI/CABG | 85.7% | Diabetes | 42.2% |
| 2 years follow up study results from International EECP Registery | |||
Long-term Benefit:
| Journal | Year | Number of patients | Result |
| American Journal of Cardiology | 1995 | 18 | 3-year survival 100% 76% event free |
| Clinical Cardiology | 2000 | 33 | 5-years survival 88% 64 % event free |
| American Journal of Cardiology | 2004 | 1097 | 2-year survival 91% 41% event free. (32% heart failure, 43% DM, prior MI 68%) |
| Long term clinical follow up study on EECP. | |||
Clinical Benefit Summary:
| Authors | Journal | N | Agina (% >/ 1CCS) | Nitrate Use | Ex. Tolerance | Time to ST Depression |
| Arora etal (MUST EECP) | JAM Coll cardiology 1999 | 139 | ||||
| Lawson et al. | Cardiology 2000 | 2238 | 74% | N/A | N/A | N/A |
| Styes et al | Angiology 2001 | 395 | 88% | N/A | N/A | N/A |
| Barsness et al | Clinical Cardiology 2001 | 978 | 88% | N/A | N/A | |
| Clinical improvement after EECP treatment N= Number of Patients = decreased, = increased, N/A = Not available |
||||||
Mechanism of action:
1. Improve Myocardial Perfusion to ischemic areaEECP has shown to improve the myocardial perfusion to the ischemic area. It is assessed by PET and SPECT Nuclear study. The Mechanism is believed to be increase pressure gradient and coronary blood flow velocity in coronary vascular bed. This will lead to formation of new vessels and opening of the dormant collaterals
| Authors | Journal | N | Agina (% >/ 1CCS) | Nitrate Use | Ex. Tolerance | Time to ST Depression |
| Arora etal (MUST EECP) | JAM Coll cardiology 1999 | 139 | ||||
| Lawson et al. | Cardiology 2000 | 2238 | 74% | N/A | N/A | N/A |
| Styes et al | Angiology 2001 | 395 | 88% | N/A | N/A | N/A |
| Barsness et al | Clinical Cardiology 2001 | 978 | 88% | N/A | N/A | |
| Clinical improvement after EECP treatment N= Number of Patients = decreased, = increased, N/A = Not available |
||||||
Patient Selection
1.Chronic CAD
Primary utilization of EECPis those who no longer respond to medication.(a) Surgery / PTCA not contemplated
Patients may not be amenable to PCI or CABG due to following:- Patients who refused for invasive procedure.
- Diffuse distal disease.
- Target lesion is inaccessible.
- LV dysfunction—High risk CABG.
- Restenosis after PTCA.
(b) Preparation for Revascularization
- Severe LV Dysfunction with lot of hibernation to Stabilize Heart Function.
- Waiting due to some other reason.
2.Heart Failure
- Non-Ischemic cardiomyopathy.
- Ischemic Cardiomyopathy.
- Patient with LV Dysfunction.
- Patient with moderate to severe levels of CHF.
3.Microvascular Angina
Cardiac syndrome X4. Acute Coronary Syndrome
- Unstable Angina.
- Acute MI.
- Cardiogenic shock.
Contraindications Check List
- Significant AR.
- DVT/active thrombophlibities.
- Congenital Heart Disease.
- Gross CHF.
- Uncontrolled arrhythmia AF, VT, Frequent VPC’s.
- Extreme Hypertension (BP>180/110mmHg).
- Extreme Tachycardia (HR>120 BPM).
- Cardiac Cath in Prior 1-2 weeks.
- Bleeding Diathesis.
- Pregnancy.
Precautions
Precautions In some patients with a history of congestive heart failure (CHF) or low ejection fraction, left ventricular function may be insufficient to compensate for increased venous return during EECP. These patients should have their fluid balance closely monitored. Cuff pressure and deflation timing should be optimized for achieving maximum after load reduction and reducing the possibility of pulmonary congestion.EECP should be withheld if there is exacerbation of heart failure symptoms and may be resumed once the patient has been stabilized. In patient with manageable edema with LVEF>35% continuous monitoring of oxygen saturation should be initiated.
Severe peripheral vascular disease including significant ileofemoral arterial obstruciton may limit the effectiveness of EECP treatment due to decreased blood flow.
Patient suspected of having an abdominal aortic aneurysm should be evaluated for its clinical significance prior to treatment with EECP.
EECP in heart failure patients
Patient with LVD with history of heart failure a course of EECP treatment has shown to decrease the Endothelin and nitric oxide ratio. This shift results in vasodilatation, which is persistent even after 3 months of completion of treatment. EECP thus benefits the patient with both ischemic and idiopathic cardiomyopathy independent of effect on Angiogenesis and collateral formation.Safety of EECP in patients with Congestive Heart failure.
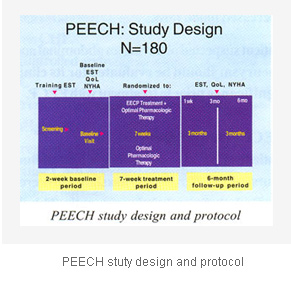
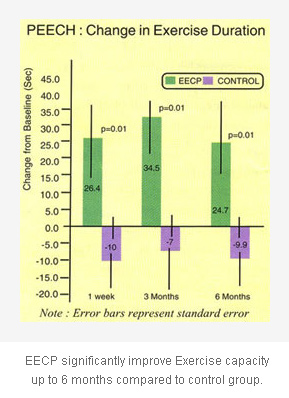
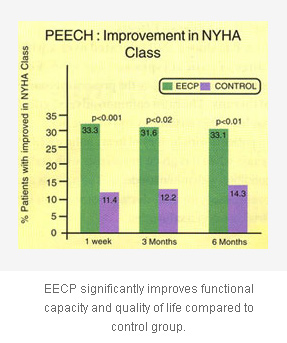
(General Cardiology 2001 Lawson et al.). During treatment only 5.5% experienced worsening of their congestive heart failure. In six months follow up study of 444 patents with history of CHF with EF less than 39%, 88% with multiple vessel disease only 19% where re-hospitalize for CHF, which is only 1/3 rd of the expected re-hospitalization when compare to other randomize study with similar patient group.PEECHTMTRIAL PROSPECTIVE EVALUATION OF EECP In Congestive Heart Failure
Conclusion:
Randomized, controlled multi center PEECH trail result supports the use of EECP treatment in heart failure patients.- EECP is well tolerated in heart failure patient
- Results suggest that EECP provides adjunctive therapy in patients with NYHA II-III heart failure receiving optimal pharmacologic therapy
Possible Adverse Effects
EECP is shown well tolerated over a wide range of patient types and age span. Few patients do not complete the prescribed course of therapy. The most common adverse effect has been skin irritations and muscle pain. In patients with history of heart failure EECP is safe when it is given to patients with stable condition with minimal edema. The patients are continuously monitor during the treatment for drop in oxygen saturation.| Clinical Summary | ||
| Clinical Improvements | Objective Improvements | Biochemical changes |
| Reduction in anginal episodes | Increases time to ST-Segment depression | Decreases in Endothelin level |
| Reduction in use of Nitrates | Increases treadmill exercise time | Increases in nitric oxide level |
| Improvement in exercise tolerance | Improves stress myocardial perfusion | Decreases oxidateive stress |
| Improvement in overall quality of life | Improves PET scan myocardial perfusion | Decreases in BNP Level |
| All outcomes sustained for longer-term | Improvement in peak oxygen consumption | Increases in VEGE level |
| Improves wall motion abnormality | ||
| Increases cardiac output | ||
| Increases ejection fraction | ||
Possible Mechanism of action to clinical improvement in Chronic angina & heart failure patients
- TMPG - Trans Myocardial Pressure gradient
- VEGF - Vascular endothelial growth factor
- HGF - Hepatocyte Growth factor
- FGF - Fibroblast Growth factor
- No - Nitric oxide
- LVEF - Left ventricular ejection fraction
- FMD - Flow mediated vasodilatation
- RH(PAT) - Reactive hyoperemia, Peripheral artery tonometer

